Merit-Based Incentive Payment System (MIPS) & QPP
Everything You Need to Secure Your Earnings
To maximize incentive payments and avoid losing money, your practice needs an EHR software with a QPP management solution and a dedicated team of attestation experts to help you out. The good news is, Meditab has both! Improve your MIPS score with us.
Powerful MIPS Tools, Unparalleled QPP Support
Meditab’s Intelligent Medical Software (IMS) is prepared to handle the new MACRA/MIPS framework, so you can seamlessly and successfully transition towards value-based care.
Unlike other EHRs, IMS supports all MIPS measures, so there’s no limit to the goals you can set for your practice. With features designed specifically for the Quality Payment Program (QPP), IMS is a perfect partner to achieving better clinical outcomes and having healthier patients.
QPP: Payment Management Software
Our Team of MIPS & QPP Experts Has Your Back
Let Us Improve Your MIPS Score
IMS offers more than just a progress tracker and an incentive calculator. In addition to our powerful QPP-specific tools, a dedicated QPP specialist will also be assigned to assist you all throughout the reporting period. We’ve got you covered from start to finish, and here’s how our QPP team does it:
Notification
We’ll let you know once you are eligible to participate in QPPs such as MIPS.
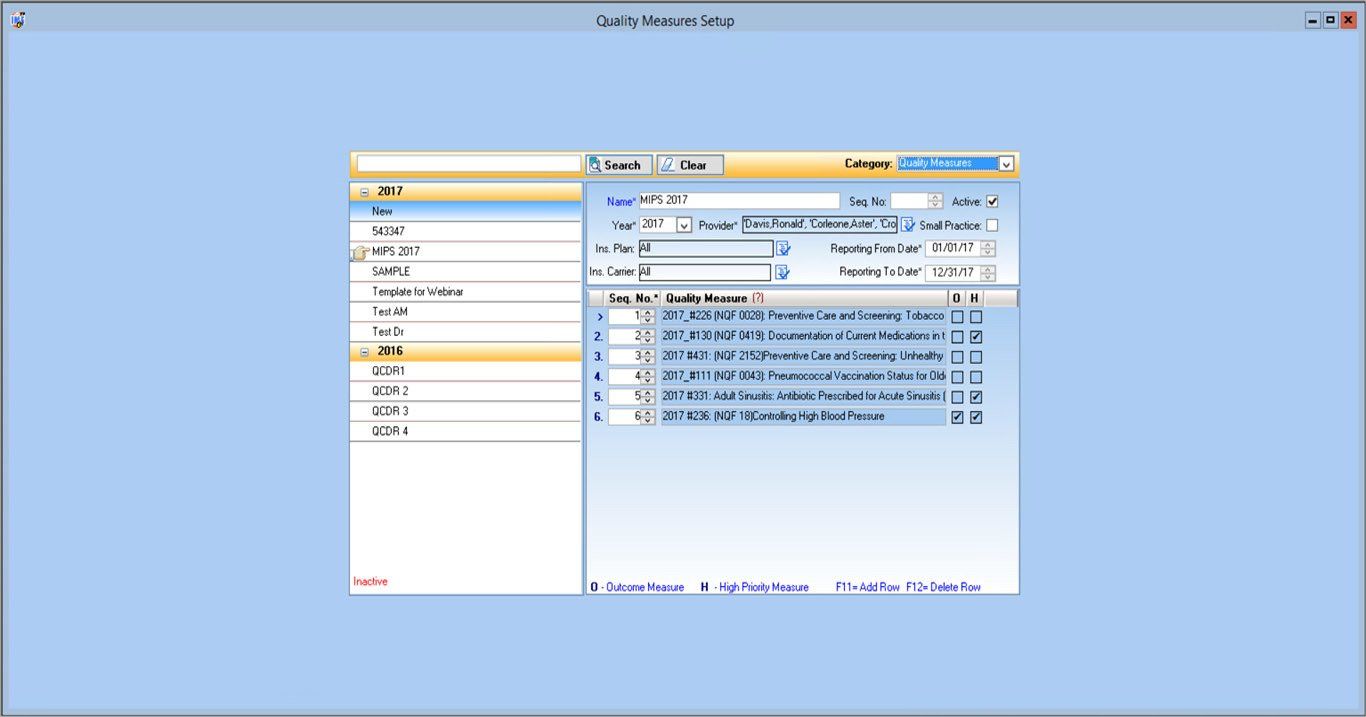
IMS setup and customization
With our team’s expertise in IMS implementation, we will set up, map, and customize the software to automate your compliance process.
Support during auditing
Should CMS decide to audit your practice, our team offers full support in providing the necessary documents to validate your report.
Assistance with validation and submission
Our job doesn’t stop when you get high scores. We will take care of running your practice data by CMS for validation. Once validated, we will even submit it through the CMS portal on your behalf.
Training and feedback
Not only will we train you and your staff on how to use IMS, we will also run regular checks to see how you are doing. We will go over your progress and provide tips on how you can get a higher MIPS score.
Assistance in determining which measures to meet
We help you choose which MIPS measures best fit your practice based on your clinic workflow, so you can reach your goals without any disruptions to your day-to-day.
Ready to know more about how Meditab can help turn QPP
into an opportunity for your success?
Your Guide to MIPS 2024
MIPS 2024
MIPS-eligible clinicians (ECs) must participate and submit their data on or before
March 31, 2025, to avoid a
9% payment penalty. Eligible clinicians, groups, and virtual groups that encountered extreme and uncontrollable circumstances may apply for an exception.
The Extreme and Uncontrollable Circumstances (EUC) exception reweights your MIPS performance categories to as low as 0%. The MIPS EUC exception application for the 2024 performance year will be available until 8 p.m. ET on December 31, 2024.
Our team of attestation experts can help you apply for the EUC exception without the hassle. To learn more about the MIPS 2024 exceptions,
click here.
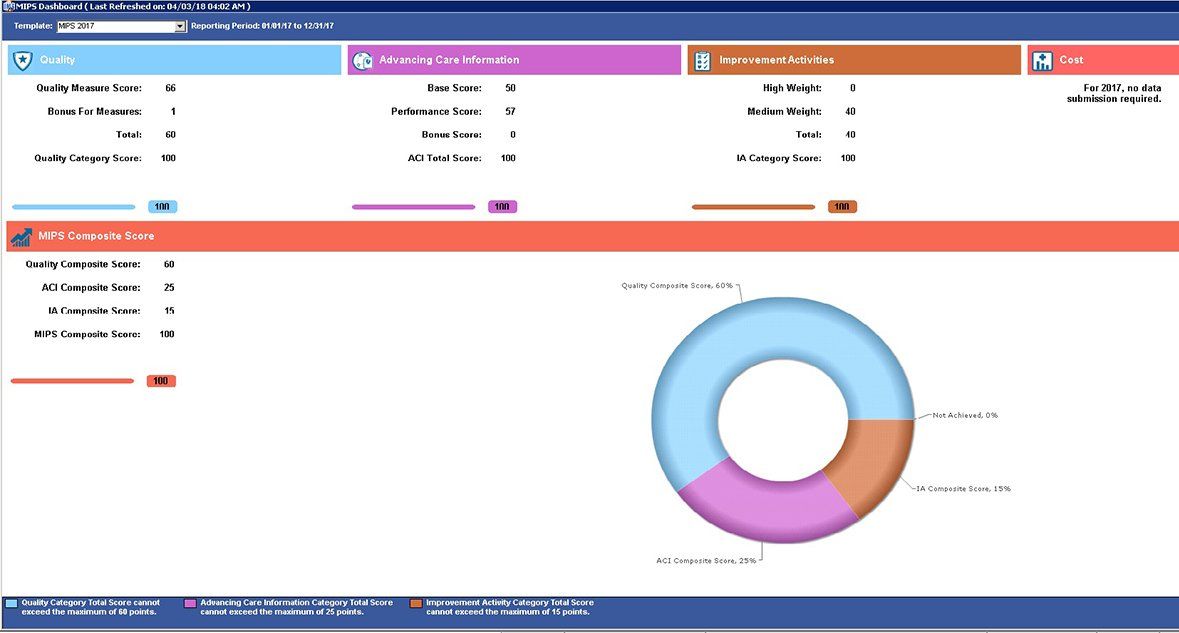
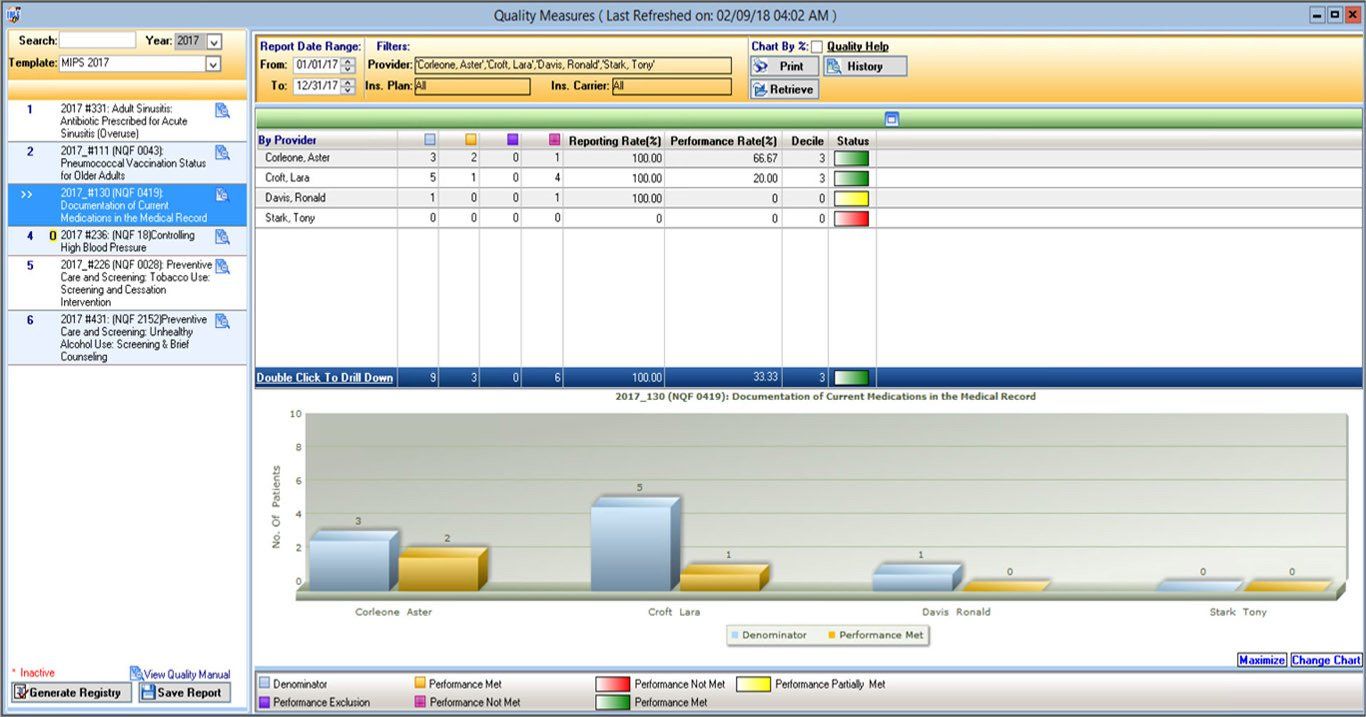
Quality Measures
The Quality performance category accounts for 30% of your final MIPS score over a 12-month performance period (January 1–December 31, 2024).
Eligible clinicians must select 6 individual measures, 1 of which must be an outcome or a high-priority measure. You may also choose to submit data for a specialty measure set that best fits your practice.
- There must be at least 20 cases per measure.
- If fewer than 6 measures apply, then you have to report on each applicable measure.
- Eligible clinicians from small practices (15 or fewer ECs) who submit data on at least 1 quality measure may qualify for the Small Practice bonus and earn 6 points.
- You can also receive up to 10 additional percentage points based on your improvement in the Quality performance category from the previous year.
Instead of the usual 70% data completeness threshold, the Centers for Medicare and Medicaid Services (CMS) now requires you to report performance data for
at least 75%
of the denominator-eligible cases for each quality measure. Measures can generally earn between 1 and 10 points based on the following:
- Your performance if the measures have a benchmark
- If you meet the 75% data completeness threshold
- If you meet the minimum requirement of 20 cases per measure
New Quality measures in their first year have a scoring floor of 7 points, while new Quality measures in their second year have a scoring floor of 5.
Measures that fail to meet the data completeness criteria receive zero points (small practices will continue to receive 3 points).
You can review the available Quality measures
here.
Cost Measures
The Cost performance category accounts for 30% of your final MIPS score over a 12-month performance period (January 1–December 31, 2024).
Qualified participants can continue to earn a 1% improvement score if they have improved their Cost performance category score from the previous year.
Beginning the 2024 performance period, the acute inpatient medical condition measure
Simple Pneumonia with Hospitalization
has been removed from the Cost performance category. On the other hand, the following new episode-based cost measures have been introduced, each with a 20-episode case minimum:
- An acute inpatient medical condition measure (psychoses and related conditions)
- 3 chronic condition measures (depression, heart failure, and low back pain)
- A measure focusing on care provided in the emergency department setting (emergency medicine)
Cost Measure Case Minimums
- Case minimum of 20 for Total per Capita Cost measure and 35 for MSPB
- Case minimum of 20 for acute inpatient medical condition episodes
- Case minimum of 10 for procedural episodes
CMS uses Medicare claims to calculate your Cost measure performance, so you don’t have to submit any data for this category.
To learn more about the Cost measures,
click here.
Promoting Interoperability
The Promoting Interoperability (PI) category accounts for 25% of your final MIPS score. Its performance period spans 180 consecutive days in the same performance year, an increase from last year’s 90-day period.
For the 2024 performance year, CMS requires you to use an electronic health record (EHR) that meets the 2015 Edition certification criteria, 2015 Edition Cures Update certification criteria, or a combination of both. You must submit collected data for specific measures from each of the 4 objectives.
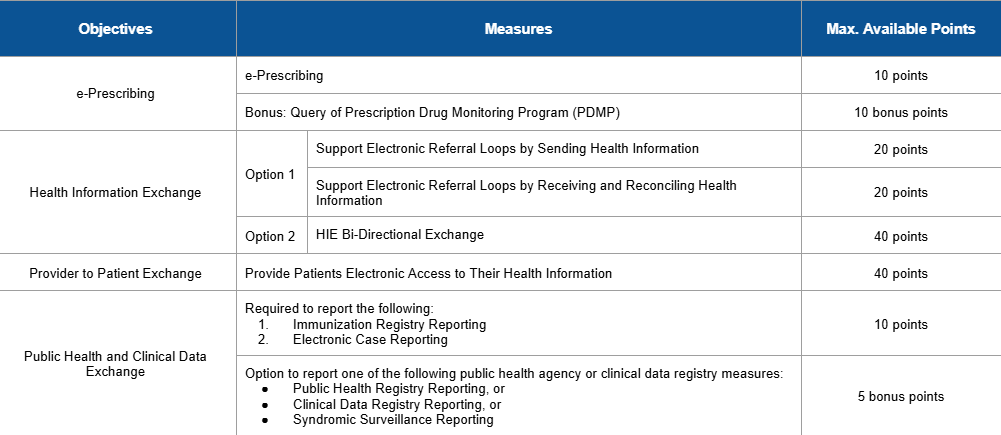
You can review the PI measures here.
To earn a score for the PI category, an eligible clinician must:
- Provide their EHR’s CMS identification code.
- Collect data in EHR technology with the 2015 Edition functionality for 180 consecutive days.
- Submit a “yes” to the Actions to Limit or Restrict Interoperability of CEHRT attestation.
- Answer the ONC Direct Review attestation. This is optional, so you may attest “yes” or “no.”
- Submit a “yes” to the Security Risk Analysis measure.
- Submit a “yes” to the new SAFER Guides attestation.
- Report the 5 to 6 required measures or claim their exclusion(s).
CMS has also exempted several clinician types from reporting PI data, including those with special status designations that result in automatic reweighting.
- Clinician Type: Clinical social workers
- Special Status: Ambulatory surgical center (ASC)-based, hospital-based, non-patient facing, and small practice
Meanwhile, physical therapists, occupational therapists, qualified speech-language pathologists, qualified audiologists, clinical psychologists, and registered dieticians or nutrition professionals are now required to report PI data.
You may apply for a MIPS Promoting Interoperability Performance Category Hardship Exception to reweight your PI measures to 0%. Learn more about the PI exception
here.
Improvement Activities
The Improvement Activities (IA) category accounts for 15% of your final MIPS score over a continuous 90-day period in the same performance year.
To earn full credit in the IA category of your 2024 MIPS reporting, you must generally submit one of the following combinations of activities:
- 2 high-weighted activities,
- 1 high-weighted activity and 2 medium-weighted activities, or
- 4 medium-weighted activities.
You can earn a maximum of 40 points for attesting to activities in the IA performance category. High-weighted activities receive 20 points, while medium-weighted activities receive 10. Meanwhile, clinicians with special statuses (i.e., small practices, HPSA providers, non-patient facing, and rural) may receive double points for each high-weighted or medium-weighted activity they submit.
Practices that are certified patient-centered medical homes (PCMH) may earn the maximum Improvement Activity performance category.
For group reporting, at least 50% of the clinicians in the group need to attest to performing the same activity during the 90-day period.
To learn more about the IA measure,
click here.
Merit-Based Incentive Payment System (MIPS) Timeline
Quality
12 months performance period
Cost
12 months performance period
Promoting Interoperability
90 Days performance period
Improvement Activities
90 Days performance period
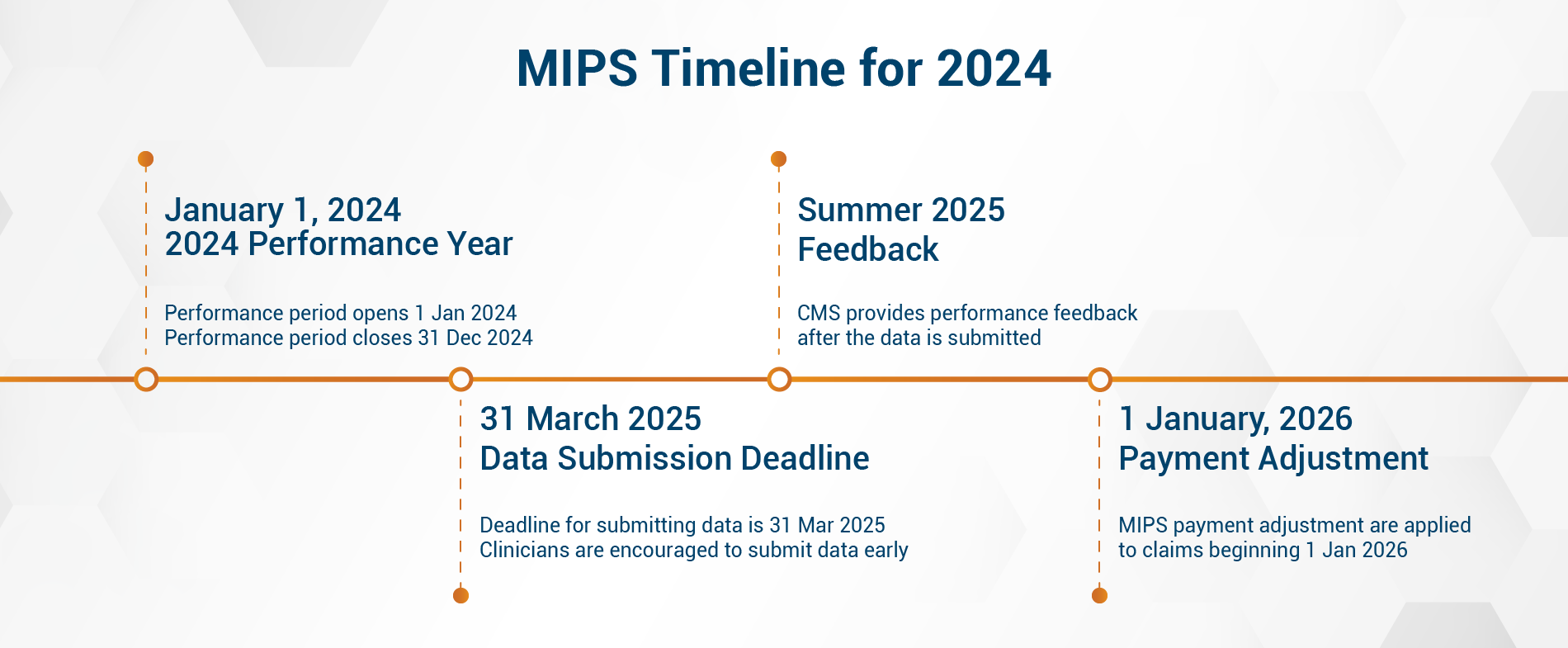
Your MIPS payment adjustment will depend on how much data you submit and your performance results. For more information, please visit https://qpp.cms.gov/.
MIPS success made possible.
Select the MIPS package that works best for you.
Plus Package
All Categories
(365 Days)
- Assist clients in choosing Quality measures applicable to their practice (at least 6).
- Education/Training on how to achieve all categories.
- Attestation for IA.
- Attestation for PI.
- Data submission for Quality.
Standard Package Quality and IA
(365 days)
- Assist client in choosing Quality measures applicable to their practice (at least 6)
- Education/Training on how to report the chosen measures
- Data validation for Quality measures
- Attestation for IA
- Data submission for the Quality measures
Standard Package Quality and PI
(365 days)
- Assist client in choosing Quality measures applicable to their practice (at least 6)
- Education/Training on how to report chosen measures
- Attestation for PI
- Data submission for Quality
Standard Package PI and IA
(90 - 365 days)
- Assist client in setup of PI and IA measures applicable to their practice
- Education/Training on how to report the chosen measures
- Attestation for IA
- Attestation for PI
What Our Clients Have to Say
“To the QPP team, I really appreciate you helping me in getting the right measures. Thank you so much, you’ve been incredibly helpful and I do appreciate it.”
Dr. Aarti Kapur,
Aarti Kapur MD PA
“Working with the IMS team on MIPS has made the entire process so much easier. They take the stress out of a process that could otherwise be extremely stressful.”